Health
Can IBS Cause Weight Gain or Weight Loss? Experts Explain
Can Irritable Bowel Syndrome (IBS) cause weight changes? Discover how IBS may lead to either weight loss or weight gain, and what you can do to manage it effectively.

Irritable Bowel Syndrome (IBS) is widely known for causing uncomfortable digestive symptoms like bloating, diarrhea, constipation, and abdominal pain—but many people wonder: Can IBS affect your weight? The answer is yes. IBS can contribute to both weight gain and weight loss, depending on the type of IBS and how it affects your eating habits, digestion, and nutrient absorption.
In this article, we break down how IBS may impact your weight, what red flags to look out for, and when to seek help from a doctor or digestive health specialist.

Can IBS Cause Weight Loss?
Yes—unintentional weight loss is possible with IBS, especially for people with IBS-D (diarrhea-predominant) or severe digestive symptoms.
Reasons IBS May Cause Weight Loss:
- Reduced appetite due to ongoing nausea, cramping, or discomfort
- Avoiding food because of fear it will trigger symptoms
- Malabsorption of nutrients, especially if you have bacterial overgrowth or chronic diarrhea
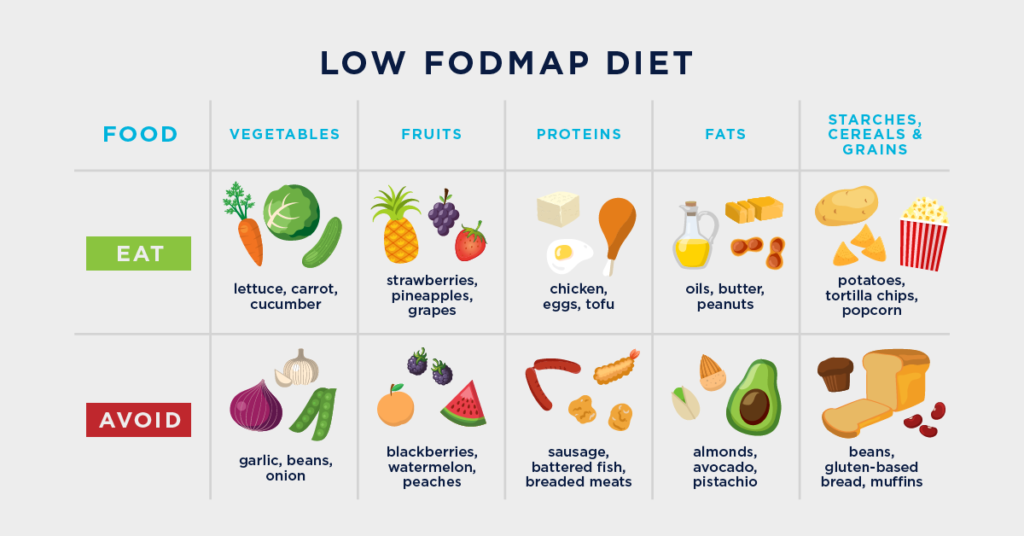
- Food restrictions, such as low-FODMAP or elimination diets, done without proper guidance
👉 Important: While mild weight changes can happen, significant or unexplained weight loss should always be evaluated. In some cases, it may be a sign of a more serious condition like Celiac disease, Crohn’s disease, or even colon cancer.
Can IBS Cause Weight Gain?
Absolutely. Many people are surprised to learn that IBS can also lead to weight gain, particularly in IBS-C (constipation-predominant) and IBS-M (mixed-type).
Reasons IBS May Cause Weight Gain:
- Constipation and bloating can lead to water retention and abdominal distension
- Eating to soothe symptoms, especially comfort foods high in sugar or fat
- Limited physical activity due to fatigue or digestive discomfort
- Slow bowel transit time, making digestion sluggish and affecting metabolism
In some cases, people may gain weight while trying to manage their symptoms with restrictive diets, processed “safe” foods, or low-fiber meals.
How to Manage Weight With IBS
Managing your weight with IBS requires a balanced approach that supports both gut health and overall nutrition.
1. Work with a specialist
A registered dietitian or IBS-focused healthcare provider can help create a customized eating plan that supports symptom relief without compromising nutritional needs.
2. Monitor your symptoms
Keep a food and symptom journal to identify potential triggers and patterns that impact your weight.
3. Choose nutrient-dense, gut-friendly foods
Focus on low-FODMAP options, cooked vegetables, lean proteins, and fermented foods if tolerated.
4. Incorporate gentle movement
Even light exercise like walking or yoga can help regulate digestion and support healthy metabolism.
5. Consider a targeted probiotic
Gut health supplements like GutShield – Liquid Spore Probiotic can help balance your microbiome, reduce bloating, and improve nutrient absorption—key factors in maintaining a healthy weight with IBS.
🟢 GutShield is designed to survive the harsh stomach environment and reach your intestines alive, where it can make a difference.
When to See a Doctor
See your healthcare provider if you experience:
- Rapid or unexplained weight loss
- Persistent weight gain despite no dietary changes
- Severe abdominal pain or changes in bowel habits
- Signs of malnutrition like fatigue, hair loss, or pale skin
An accurate IBS diagnosis and ruling out other conditions are crucial before starting any treatment plan.
Takeaway
So, can IBS cause weight gain or weight loss? Yes—it can do both, depending on how it affects your body. Weight changes with IBS are common but often misunderstood. The good news is that with the right approach—including nutrition, lifestyle changes, and expert support—you can get your symptoms and your weight under control.
Health
Tricks the Medical System Plays on You: Understanding Causes vs. Symptoms
The medical system is one of the most successful business models ever created. It generates trillions of dollars every year, making it both incredibly lucrative and, in some ways, deeply manipulative.

The medical system is one of the most successful business models ever created. It generates trillions of dollars every year, making it both incredibly lucrative and, in some ways, deeply manipulative. On this Halloween, let’s unravel the spooky trick it plays—confusing causes with symptoms—to keep you focused on the wrong things and selling you solutions that often don’t address the root of your problems.
Symptoms vs. Causes: Can You Tell the Difference?
Let’s start with a test:
Is IBS a symptom or a cause?
What about fatigue, joint pain, or headaches?
Crohn’s disease? Ulcerative colitis? Slow gut motility? Gastroparesis?
The answer is simple: all of these are symptoms. Not one of them is a cause. Yet, many people believe they are causes because the medical system—and even reputable books and websites—present them that way.
Doctors often label a condition or syndrome as the “cause” of your health problems without asking the essential question: What caused that condition in the first place? While genetics may play a role in rare cases, there is almost always an underlying cause that needs to be uncovered.
How the System Sells You Your Symptoms
Let’s look at a common example: chronic constipation.
When someone with chronic constipation visits their doctor, they might get an abdominal x-ray. The x-ray shows stool backed up in the colon, and the doctor points to it, saying, “Here’s your problem. You need to clear out this stool. Take this medication.”
On the surface, this might seem reasonable. But let’s break it down.
Of course, stool is backed up in the colon—that’s literally the definition of constipation.
The x-ray is simply showing the symptom, not the cause.
The real issue is why the stool is backed up in the first place. That’s the cause, and addressing it is the only way to solve the problem for good.
IBS: A Diagnosis Without Answers
Irritable Bowel Syndrome (IBS) is another example of how the medical system misleads. IBS is not a cause—it’s a broad label for a collection of digestive symptoms that doctors don’t know how to address.
Every day, researchers search for a cure for IBS, but they’ll never find it. Why? Because IBS isn’t a disease or a single symptom—it’s a label for hundreds of potential underlying causes.
At the IBS Doctor ORG, we focus on identifying these causes. And we know we’ve found the root issue because the symptoms disappear when the cause is addressed. Not only that, but other health issues often improve as well.
How to Know If You’re Treating the Cause
Here’s a simple way to determine if you’re addressing the cause of your condition:
If you stop treatment and the symptoms return, you’re likely treating the symptom, not the cause.
Medications, including painkillers, often mask symptoms without solving the underlying problem.
When you eliminate the cause, symptoms go away for good, and your overall health improves. That’s the power of addressing the root issue.
A Never-Ending Cycle of New Conditions
Causes are finite, but the medical system thrives on creating infinite new conditions. For as long as there’s money to be made, new labels and syndromes will continue to emerge, ensuring there’s always something to sell.
The Bottom Line: Always Question
No matter what chronic condition, syndrome, or disease you’re dealing with, ask yourself: Am I addressing the cause or just managing the symptom?
The path to true healing lies in identifying and treating the cause. Don’t settle for a system that sells you your symptoms. Demand more, dig deeper, and take control of your health.
Health
How To Break Biofilms
Biofilms are a significant obstacle in effectively treating Candida or bacterial overgrowth in the digestive tract.

Biofilms are a significant obstacle in effectively treating Candida or bacterial overgrowth in the digestive tract. If you’ve struggled with treatments that seem to work temporarily but fail in the long term, biofilms may be the culprit. Here’s what you need to know about biofilms, how they interfere with treatment, and what you can do to overcome this challenge.
What Are Biofilms?
Biofilms are thin layers of biological material formed by bacteria or yeast, such as Candida, in the lining of the digestive tract. These colonies create layer upon layer of microbial cells, which secrete a protective slimy coating made of natural polymers.
The longer bacteria or Candida remain in your digestive system, the more time they have to develop these biofilms, creating a robust barrier that protects them from treatment.

How Biofilms Interfere with Treatment
The protective layer of a biofilm prevents antibiotics, antifungals, or natural supplements from reaching the bacteria or yeast inside. This barrier significantly reduces the effectiveness of your treatment.
Here’s how it impacts your recovery:
- Incomplete Treatment: Your medication or supplement may only affect the outermost layers of the biofilm, leaving the bacteria or yeast deeper inside untouched.
- Recurring Problems: Even if you experience temporary relief, the remaining organisms can “reseed” themselves, causing the overgrowth to return.
- Frustrating Cycles: Many people follow their treatment plan diligently but find that their symptoms persist or keep coming back because the biofilm was never addressed.
How to Treat Biofilms
To successfully treat Candida or bacterial overgrowth, it’s essential to target the biofilm while addressing the root infection.
Steps to Break Down Biofilms
- Use a Biofilm Disruptor:
- A biofilm disruptor works to break down the polysaccharide layer that protects the organisms within the biofilm.
- For years, at the IBS Treatment Center, we’ve used Dr. Wangen’s Biofilm Pro, a product specifically designed for this purpose.
- Timing Is Key:
- Take the biofilm disruptor on an empty stomach to prevent it from interacting with food.
- Wait at least an hour after taking the disruptor before starting your Candida or bacterial treatment. This timing ensures that the biofilm is weakened, allowing your treatment to reach the target organisms effectively.
- Follow the Directions:
- Consistency is crucial. Follow the instructions on the bottle carefully to maximize the disruptor’s effectiveness.

Where to Get Biofilm Pro
You can purchase Dr. Wangen’s Biofilm Pro directly from the IBSDOCTOR.ORG. Visit our website at www.IBSDoctor.ORG or check the link in the pinned comment below to get started.
The Benefits of Treating Biofilms
Addressing the biofilm layer allows your treatment to work as intended, helping you achieve:
- More Effective Symptom Relief: Eliminate the root cause rather than just the surface symptoms.
- Long-Term Results: Prevent the overgrowth from recurring by fully eradicating the bacteria or Candida.
- Improved Overall Health: A cleaner, healthier gut contributes to better digestion and overall well-being.
Conclusion: Get Over the Hump
Biofilms are a hidden but significant barrier to successful treatment for Candida and bacterial overgrowth. By addressing the biofilm directly, you can unlock the full potential of your treatment plan and achieve lasting results.
Don’t let biofilms hold you back—take control of your gut health today!
Health
4 Things You Need to Know About Calprotectin
Calprotectin is a common marker included in stool tests, but there’s significant misinformation surrounding what it indicates about your digestive health.

Calprotectin is a common marker included in stool tests, but there’s significant misinformation surrounding what it indicates about your digestive health. Here’s a clear breakdown of what calprotectin can—and cannot—tell you about your colon, based on years of clinical experience testing calprotectin levels in thousands of patients.
What Is Calprotectin?

Calprotectin is a protein expressed by various cells in the body, particularly those involved in the immune system. As such, it’s considered an inflammatory marker since it’s associated with immune responses and inflammation.
You may have heard that calprotectin is primarily used to differentiate between Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS), but the reality is far more nuanced.
Does Calprotectin Differentiate Between IBD and IBS?
The short answer: not reliably.
- While elevated calprotectin levels are more commonly associated with IBD, I’ve seen plenty of IBS patients with elevated calprotectin levels who don’t have IBD.
- Many of these IBS patients had undergone colonoscopies that definitively ruled out IBD, showing that calprotectin alone isn’t a definitive diagnostic tool.
Calprotectin may have some correlation with IBD, but it isn’t specific or sensitive enough to be a standalone marker for distinguishing between IBD and IBS.
Calprotectin Is One Inflammatory Marker, Not the Only One
Inflammation is incredibly complex, and calprotectin is just one of many markers that may indicate it.
- Not the Whole Picture: No single test can comprehensively measure inflammation in the body, including in the digestive tract. While calprotectin is a helpful tool, it doesn’t provide the full story.
- Variability in Inflammation: The presence of inflammation can be influenced by numerous factors, and other markers may be more relevant in specific cases.
Calprotectin Is Also Produced by Epithelial Cells
Another key fact about calprotectin is that it’s not solely produced by immune cells.
- Epithelial Cells: These cells line the digestive tract and other parts of the body, and they can also produce calprotectin.
- Misleading Associations: Elevated calprotectin levels might not always be tied to immune-related inflammation. Instead, the elevation could stem from epithelial cell activity, making the interpretation of results more complex.
What Does an Elevated Calprotectin Level Mean?
An elevated calprotectin level is not specific to any one condition. Here’s what you need to know:
- It’s a Monitoring Tool, Not a Diagnostic Marker:
- Calprotectin levels can be useful for tracking changes over time, especially to evaluate how well a treatment is working.
- For example, a decrease in calprotectin levels might indicate that your treatment is reducing inflammation or addressing the issue effectively.
- It Doesn’t Identify the Cause:
- Elevated calprotectin levels don’t tell you why it’s elevated. The marker doesn’t point to a specific diagnosis or underlying condition.
The Bottom Line on Calprotectin

Calprotectin is a valuable tool, but it has limitations. Here’s a quick summary:
- What It Does: Helps monitor inflammatory activity and evaluate treatment effectiveness.
- What It Doesn’t Do: Diagnose specific conditions, reliably differentiate between IBD and IBS, or provide a complete picture of inflammation.
- If you’ve had calprotectin levels tested, it’s crucial to interpret the results within the broader context of your symptoms, other diagnostic tests, and clinical findings. Always consult with a knowledgeable healthcare provider to understand what your calprotectin levels mean for your unique situation.
- By understanding the nuances of calprotectin, you can approach your digestive health with clarity and informed decision-making.
-
 Health8 năm ago
Health8 năm agoAll About Microscopic Colitis: Causes, Diagnosis, and Treatment
-

 Health8 năm ago
Health8 năm agoWhat Causes Mucus in Your Stool—and Why You Shouldn’t Ignore It
-

 Health8 năm ago
Health8 năm agoWhat Is a Gastroenterologist? When to See One, and the Problems They Can’t Help With
-

 Entertainment8 năm ago
Entertainment8 năm agoI Tried Medication, Diets, and Meditation — And Finally Found Peace in Acceptance
-

 Health8 năm ago
Health8 năm agoTop 7 Questions to Ask Your Gastroenterologist!
-

 Health8 năm ago
Health8 năm agoA New Cause and Treatment for Lymphedema
-

 Health8 năm ago
Health8 năm agoHow Pseudomonas Can Impact Your IBS: What You Need to Know
-

 Business8 năm ago
Business8 năm ago“I’m Not Lazy — I’m Surviving an Invisible Illness”: Understanding the Daily Struggle of Living with IBS













