Health
The IBS-Friendly Morning Routine That Can Calm Your Gut All Day
Your morning choices can set the tone for your gut health all day. Discover a simple, IBS-friendly routine that supports the gut-brain axis, reduces inflammation, and promotes comfortable digestion.

What if the way you start your morning could determine whether you spend the rest of your day in comfort—or in pain?

For people with Irritable Bowel Syndrome (IBS), mornings can feel like a gamble. One wrong choice—whether it’s a cup of strong coffee on an empty stomach or skipping breakfast entirely—can trigger bloating, cramps, or urgent bathroom trips that last all day.
Emerging research shows that morning routines influence the gut-brain axis, the two-way communication system between your digestive tract and nervous system. This axis controls motility (how food moves through your intestines) and regulates inflammation—both of which are key players in IBS.
A calm, balanced start can keep your gut in “rest and digest” mode rather than fight-or-flight, reducing the likelihood of flare-ups.
Your IBS-Friendly Morning Blueprint

1️⃣ Drink Warm Water Before Anything Else
Hydration supports smooth bowel movements and helps “wake up” the digestive tract without the jolt of caffeine. Warm water can be especially soothing for intestinal muscles.
2️⃣ Practice 5 Minutes of Deep Breathing
Deep, diaphragmatic breathing activates the parasympathetic nervous system, which encourages healthy digestion and reduces gut hypersensitivity. Try inhaling for 4 counts, holding for 4, and exhaling for 6.
3️⃣ Have a Gentle, Protein-Rich Breakfast with Soluble Fiber
Instead of skipping breakfast or eating ultra-processed carbs, choose:
- Soft scrambled eggs with a side of cooked oats
- Smoothie with lactose-free yogurt, chia seeds, and banana
Soluble fiber from oats or chia seeds helps regulate bowel movements, while light protein stabilizes blood sugar and supports muscle repair.
4️⃣ Avoid Caffeine First Thing
Coffee immediately after waking can overstimulate the gut and worsen diarrhea in IBS-D, or cause cramping in IBS-M. If you enjoy coffee, try having it after your breakfast to lessen the impact.
Why This Works for IBS
- Hydration + soluble fiber = easier, more regular bowel movements
- Deep breathing = calmer gut-brain signaling
- Balanced breakfast = steady energy without blood sugar spikes
- Delayed caffeine = reduced gut motility shocks and inflammation risk
Over time, these habits can train your body to start the day in digestive balance—meaning fewer flare-ups and more freedom to enjoy your day.

Start tomorrow with these small changes—and discover how calm your gut can be. Pair it with GutShields to support your microbiome from the inside out.
Health
Hydration Hacks for IBS: The Right Way to Drink Water
Drinking water the wrong way can worsen IBS symptoms. Discover how to hydrate smarter—small sips, steady timing, and natural add-ins—to support digestion and gut balance.

“It’s not just about drinking more water—it’s about drinking the right way.”
If you have Irritable Bowel Syndrome (IBS), you’ve probably been told to drink plenty of water. But here’s the catch: how you drink matters just as much as how much you drink.
For many people with IBS, chugging large amounts of water in one go can actually trigger strong intestinal contractions, leading to urgency, bloating, or discomfort.

The Science of Hydration and Digestion
- Rapid intake of water can overstimulate the digestive tract and speed up motility.
- Even, steady hydration supports smoother digestion and nutrient absorption.
- Proper hydration also helps regulate stool consistency, easing both IBS-C (constipation) and IBS-D (diarrhea).
In short: your gut doesn’t just want more water—it wants consistent hydration.
Practical Hydration Habits for IBS
Here are science-backed ways to drink water that keep your digestion steady:
✅ Sip, don’t chug
Aim for 150–200 ml (about half a cup) every 2 hours instead of gulping down large amounts at once.
✅ Infuse with digestion-friendly add-ins
A slice of lemon, cucumber, or fresh mint can make hydration enjoyable and may help soothe bloating.
✅ Match timing with meals
Drink water between meals rather than during them to reduce the risk of overwhelming your stomach acid and slowing digestion.
✅ Choose temperature wisely
Many people with IBS find that room-temperature or warm water is gentler on the gut than ice-cold water.
The Bigger Picture

Hydration is one piece of the IBS puzzle. Pairing good hydration habits with microbiome support—such as spore-based probiotics like GutShields—creates a powerful daily foundation for calmer digestion.
Bottom Line
When it comes to IBS, hydration isn’t just about volume—it’s about rhythm. Steady, mindful sipping can keep your gut balanced and your symptoms calmer.
✨ Stay hydrated, stay balanced—let GutShields help protect your gut microbiome.
Health
Why Sleep Quality Can Make or Break Your IBS Recovery
Poor sleep doesn’t just cause fatigue—it can worsen IBS by raising cortisol, triggering inflammation, and disrupting gut bacteria. Learn how to improve sleep to support your digestion and long-term gut health.

“Poor sleep isn’t just making you tired—it might be keeping your gut inflamed.”
Living with Irritable Bowel Syndrome (IBS) means constantly balancing stress, diet, and lifestyle to avoid flare-ups. But one factor often overlooked is sleep quality. Many people with IBS report that their symptoms are worse after nights of poor sleep. Science now shows this isn’t just coincidence—sleep has a direct influence on the gut-brain axis, the microbiome, and inflammation levels.
If you’ve tried dietary changes, supplements, and even medication without lasting relief, improving your sleep could be the missing piece of your IBS recovery.

The Science: How Sleep and IBS Are Connected
- Cortisol and inflammation
- Poor or fragmented sleep raises cortisol, your body’s main stress hormone.
- Elevated cortisol has been linked to increased gut permeability (“leaky gut”), more inflammation, and heightened pain sensitivity—all of which make IBS symptoms worse.
- Gut microbiome disruption
- Studies show that even short-term sleep deprivation reduces microbial diversity.
- A disrupted microbiome may lead to more gas, bloating, constipation, or diarrhea in IBS patients.
- Gut-brain axis imbalance
- Your digestive tract has its own nervous system (the enteric nervous system).
- Poor sleep dysregulates this system, which can throw off motility—causing irregular bowel habits, urgency, or spasms.
In short, sleep doesn’t just recharge your brain—it recharges your gut.
Practical Steps for IBS-Friendly Sleep

Here’s how you can start improving sleep quality—and by extension, your digestion:
✅ Set a consistent bedtime and wake time
Your circadian rhythm influences gut motility. Going to bed and waking up at the same time each day helps regulate bowel function.
✅ Limit screens at night
Blue light from phones and laptops suppresses melatonin, making it harder to fall asleep. Try switching to a book or listening to calming music.
✅ Create a wind-down ritual
Deep breathing, light stretching, or journaling can signal your nervous system to shift into “rest and digest” mode—essential for people with IBS.
✅ Support with natural aids
Chamomile tea, magnesium glycinate, or lavender aromatherapy have been shown to improve relaxation and sleep quality.
✅ Feed your microbiome wisely
Avoid late-night heavy meals, alcohol, or excess caffeine. Pair your routine with spore-based probiotics like GutShields to support a resilient microbiome overnight.

The Bigger Picture: Sleep as IBS Medicine
When you consistently improve your sleep, you’re not just preventing fatigue—you’re:
- Calming inflammation
- Helping good bacteria thrive
- Regulating gut-brain communication
- Supporting more regular, pain-free bowel movements
That’s why sleep isn’t just a lifestyle tip—it’s a therapeutic tool for IBS recovery.
Bottom Line
If you’ve been treating IBS only through diet or medication but ignoring your sleep, you may be missing a key part of the solution. By protecting your nights, you protect your gut.
✨ Give your gut the rest it deserves—combine better sleep with GutShields for faster, lasting relief.
Health
Why Sleep Is the Secret Weapon Against IBS
Struggling with IBS symptoms despite eating right? Discover how improving your sleep can significantly reduce digestive flare-ups and support gut healing.


When managing Irritable Bowel Syndrome (IBS), most people focus heavily on food. What to eat. What not to eat. Low FODMAP this, dairy-free that. But what if we told you there’s another, often overlooked, factor that plays a powerful role in your digestive health?
👉 Sleep.
Yes — your sleep habits may be silently shaping the course of your IBS journey more than you realize.
🧠 The Gut-Brain-Sleep Connection

Your digestive system and nervous system are deeply intertwined. The gut-brain axis, a bidirectional communication network between the brain and gastrointestinal (GI) tract, is profoundly influenced by sleep quality.
During restful sleep, especially deep sleep stages, your body carries out crucial healing processes:
- Reduces inflammation in the GI tract
- Supports microbiome balance
- Regulates stress hormones like cortisol
- Improves motility (the movement of food and waste through the gut)
Poor sleep, on the other hand, disrupts these processes, leading to increased sensitivity, irregular bowel movements, and a greater risk of flare-ups.
💤 Scientific Evidence: IBS and Sleep Disorders
A growing body of research supports this connection:
- Up to 70% of people with IBS report poor sleep quality or sleep disturbances
- Those with fragmented sleep have higher reports of abdominal pain, bloating, and urgency
- Poor sleep exacerbates anxiety and depression, both of which can worsen IBS symptoms
In fact, some studies suggest that addressing sleep problems can improve IBS symptoms even without changing the diet.
🌙 How to Improve Sleep for Better Digestion
Here are 6 digestive-friendly sleep tips backed by science:
- Stick to a consistent sleep schedule – helps regulate the body’s internal clock and digestive rhythm
- Create a wind-down routine – reduce blue light, heavy meals, or stressors before bed
- Limit caffeine and nicotine – stimulants can disrupt sleep and irritate the gut
- Address nighttime reflux or discomfort – elevate your head and avoid eating within 2-3 hours of bedtime
- Try spore-based probiotics – some strains like Bacillus coagulans may promote not just digestion, but improved sleep quality via gut-brain signaling
- Track your sleep and symptoms – journaling can reveal patterns between poor sleep and flare-ups
🧩 IBS Requires a Holistic Approach
Food matters. Supplements help. But healing from IBS also means rebuilding your body’s ability to regulate itself — and sleep is a cornerstone of that regulation.
When you’re well-rested, your gut is calmer. Your immune system is less reactive. Your nervous system is more resilient. The result? Fewer flares, less pain, and more freedom.
Final Thoughts
If you’ve tried all the diets, all the pills, and all the probiotics, but still struggle — it might be time to ask:
“Am I sleeping enough, and is it quality sleep?”
Because sometimes, the simplest habit — like getting a good night’s rest — can be your most powerful tool in reclaiming your health.
-
 Health8 năm ago
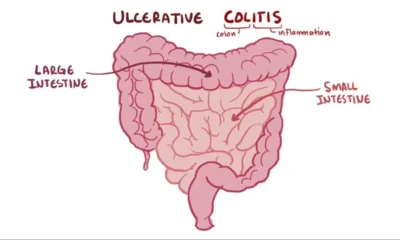
Health8 năm agoAll About Microscopic Colitis: Causes, Diagnosis, and Treatment
-

 Entertainment8 năm ago
Entertainment8 năm agoI Tried Medication, Diets, and Meditation — And Finally Found Peace in Acceptance
-

 Health8 năm ago
Health8 năm agoWhat Is a Gastroenterologist? When to See One, and the Problems They Can’t Help With
-

 Health8 năm ago
Health8 năm agoTop 7 Questions to Ask Your Gastroenterologist!
-

 Health8 năm ago
Health8 năm agoWhat Causes Mucus in Your Stool—and Why You Shouldn’t Ignore It
-

 Health8 năm ago
Health8 năm agoA New Cause and Treatment for Lymphedema
-
 Health8 năm ago
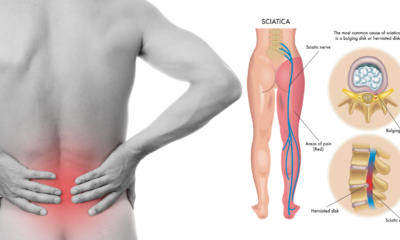
Health8 năm agoIBS and Sciatica Pain – Is There a Connection?
-

 Tech8 năm ago
Tech8 năm agoHealing IBS Isn’t About Forcing Your Gut—It’s About Resetting Its Natural Rhythm

















