Entertainment
What I Eat in a Day to Keep My IBS From Taking Over
Curious what someone with IBS eats in a day? Explore a gentle, low-trigger routine that’s realistic, gut-friendly, and actually enjoyable.


Morning: Starting Slow & Soothing
☕ Warm Water + Peppermint Tea
I begin the day with a glass of warm water and peppermint tea. Peppermint naturally helps calm the gut and eases morning cramps or urgency.
🥣 Light Breakfast – Rice Porridge with a Dash of Salt & Boiled Egg
Rather than rushing into fibrous or cold food, I keep it gentle:
- ½ cup of soft-cooked jasmine rice with warm water (like a congee)
- One soft-boiled egg for protein
💡 Why it works: Easy to digest, low-FODMAP, and comforting on sensitive mornings.
Mid-Morning Snack (Optional)
🍌 Half a Ripe Banana or a Small Handful of Peeled Papaya
If I feel hungry before lunch, I go for low-fiber fruits that don’t ferment too much.
💡 Tip: Some days, I skip snacks. IBS isn’t just about food—it’s also about stress. So I listen to my body without pressure.
Lunch: Balanced & Bloat-Free
🍗 Protein + Gentle Carbs + Cooked Veggies

- Grilled or air-fried chicken breast (no heavy spices, just salt and thyme)
- ¾ cup cooked jasmine rice or mashed potato
- Cooked zucchini or peeled carrot (steamed)
Drink: Room temperature water—no cold soda or juice that shocks the gut.
💡 Why it helps: Light but satisfying. Cooking veggies reduces fiber harshness. The meal avoids common triggers like garlic, onions, and dairy.
Afternoon Reset
🍵 Gut-Friendly Boost: Probiotic Drink or Capsule
I usually take my spore-based probiotic (like GutShields or Bacillus coagulans SNZ 1969®) about 20 minutes before dinner. This helps reinforce balance and support immune regulation without bloating.
Dinner: Light & Kind to the Gut

🥘 Soup-Based Meal – Chicken Broth with Soft Rice Noodles and Tofu
- Clear bone broth base (homemade or low-sodium)
- Silken tofu or soft chicken pieces
- A few cooked spinach leaves or grated zucchini
- Rice noodles (avoid wheat/gluten unless tested and tolerated)
💡 My rule: Nothing fried. Nothing raw. Keep it warm, soupy, and small.
Evening (If Hungry):
🧉 Chamomile or Ginger Tea + 1–2 Rice Crackers with a Spoon of Peanut Butter
If I need something, it’s gentle. I avoid chocolate, dairy, and heavy late-night carbs.
Final Notes: This Isn’t Perfection—It’s Peace
I don’t count calories. I don’t aim to be perfect. Some days I eat more, some less. What matters is that my gut feels safe, not under attack. I’ve found that consistency, calm eating, and tuning in to my own rhythm helps me stay in control without fear.
You don’t have to eat exactly like me—but if you feel stuck or overwhelmed, maybe this simple guide gives you a place to begin.
Entertainment
The #1 Cause of Hypoglycemia: What Most Doctors Overlook
Hypoglycemia is one of those frustrating conditions where patients often know more about their symptoms than their doctors.

Hypoglycemia is one of those frustrating conditions where patients often know more about their symptoms than their doctors. If you’ve struggled with hypoglycemia, you’re probably familiar with the sudden crashes, the irritability, and the desperate need to eat every couple of hours just to feel normal.
Despite how common these experiences are, the medical system rarely offers a satisfying answer—or an effective solution. But after over 25 years of working with patients (and having personally experienced hypoglycemia myself), I’ve found that the root cause of hypoglycemia is often linked to digestion.
Let’s explore why your digestive health may be the missing piece in solving your blood sugar crashes.

What Is Hypoglycemia?
Hypoglycemia refers to low blood sugar levels, but not everyone who experiences it will show abnormal readings on a lab test. Many people with hypoglycemia “just know” when it’s happening—they feel weak, shaky, lightheaded, anxious, or irritable if they go too long without eating.
For some, this means needing to eat every two hours just to function normally. Others may experience sudden crashes in energy after meals, leading to intense cravings for sugar or carbohydrates to stabilize their blood sugar again.
But why does this happen in the first place?
How Digestion Affects Blood Sugar Levels
Most people (including many doctors) assume that hypoglycemia is a purely metabolic issue. But in my experience, poor digestion and nutrient absorption are some of the biggest contributors to hypoglycemia.

Here’s why:
- If you don’t properly digest your food, you can’t extract enough nutrients from it.
- Without adequate nutrients, your body struggles to maintain stable blood sugar levels.
- As a result, your blood sugar drops faster, making you feel weak, hungry, and irritable.
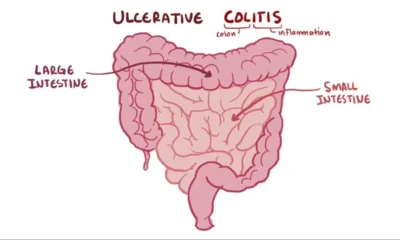
This is why people with IBS (Irritable Bowel Syndrome), chronic diarrhea, constipation, or other digestive disorders often suffer from hypoglycemia. Even if they eat plenty of food, their bodies aren’t fully absorbing the nutrients they need to sustain balanced energy levels.
Personal Experience: From Hypoglycemia to Healing
or most of my youth and into my 30s, I had severe hypoglycemia. I had to eat constantly just to feel normal. People told me I had a “fast metabolism,” but in reality, I was dealing with undiagnosed malabsorption.
At the time, I also had IBS and frequent diarrhea. My digestive system was in rough shape, but I didn’t realize how bad it was until I started healing.
As I treated my IBS and my digestion improved, something amazing happened—my hypoglycemia disappeared.
- I no longer needed to eat every two hours.
- I stopped feeling shaky or irritable if I skipped a meal.
- I could go long stretches without food and simply feel normal hunger, not panic-inducing blood sugar crashes.
Over the years, I’ve seen this happen for countless patients as well. When they heal their gut, their blood sugar stabilizes—even if they don’t have obvious digestive symptoms.
Hidden Digestive Issues That Can Cause Hypoglycemia

Even if you don’t have noticeable gut problems, your digestion may still be affecting your blood sugar levels. Here’s why:
1. “Silent” Malabsorption Conditions
Not everyone with poor digestion has obvious digestive symptoms.
For example, celiac disease (a severe reaction to gluten) often causes nutrient malabsorption even in people who don’t have stomach issues.
Many people with undiagnosed celiac disease struggle with low blood sugar, fatigue, and constant hunger because their body isn’t absorbing nutrients properly. Once they remove gluten and allow their gut to heal, their blood sugar stabilizes.
But gluten isn’t the only culprit—there are hundreds of other causes of poor digestion and malabsorption.
2. IBS, SIBO, and Gut Dysbiosis
Conditions like IBS, SIBO (Small Intestinal Bacterial Overgrowth), or an imbalance in gut bacteria (dysbiosis) can prevent your body from absorbing key nutrients. This makes it harder for your system to regulate blood sugar levels.
For example:
- Chronic diarrhea flushes out nutrients before they can be absorbed.
- Bacterial imbalances interfere with proper digestion and blood sugar regulation.
- Constipation slows metabolism and disrupts normal nutrient absorption.
3. Candida and Yeast Overgrowth
Many people with hypoglycemia crave sugar constantly—and it’s not just because of blood sugar swings. In some cases, Candida (yeast) overgrowth in the gut may be playing a role.
Candida thrives on sugar and can actually contribute to blood sugar crashes by altering how your body processes carbohydrates.
How to Fix Hypoglycemia by Healing Your Gut
If you’re struggling with hypoglycemia, treating the root cause is the key to long-term relief. Here’s where to start:
1. Identify and Treat Underlying Gut Issues
- Get tested for celiac disease, food sensitivities, SIBO, and gut dysbiosis.
- Address IBS, chronic diarrhea, or constipation to improve nutrient absorption.
- Reduce inflammation in the gut with an anti-inflammatory diet.
2. Support Blood Sugar Stability with Balanced Nutrition
- Prioritize protein, healthy fats, and fiber at every meal.
- Avoid refined sugars and processed carbs that cause rapid blood sugar swings.
- Try small, frequent meals while your gut is healing.
3. Restore Gut Health with Targeted Probiotics
One of the best ways to support digestion and nutrient absorption is by using a high-quality probiotic—specifically, a spore-based probiotic.
Liquid Spore Probiotics from GutShields are uniquely designed to:
✔ Survive stomach acid and reach the intestines alive.
✔ Support a balanced gut microbiome for better digestion.
✔ Improve nutrient absorption, which may help stabilize blood sugar.
✔ Reduce gut inflammation that could be contributing to hypoglycemia.
Unlike traditional probiotics, GutShields’ Liquid Spore Probiotics are formulated to rebuild gut health from the inside out. If you’re struggling with hypoglycemia, IBS, or digestive issues, addressing your microbiome could be the missing piece.
Final Thoughts: You CAN Fix Hypoglycemia

If you’ve been battling low blood sugar crashes, constant hunger, or the need to eat every two hours, know that there’s hope.
Hypoglycemia isn’t just about eating more—it’s about absorbing nutrients better.
By healing your gut, balancing your microbiome, and restoring proper digestion, you can finally break free from hypoglycemia and regain control of your energy levels.
Are you ready to restore your gut and take back your health? Try Liquid Spore Probiotics from GutShields today and experience the difference a healthy microbiome can make.
Entertainment
I Tried Medication, Diets, and Meditation — And Finally Found Peace in Acceptance
Living with IBS can feel like an endless cycle of treatments and hope. But for some, real healing begins not with control — but with compassion and acceptance.

If you’re living with Irritable Bowel Syndrome (IBS), you’ve likely been on the same journey I have: searching for answers, one solution at a time.
I tried medication.
I tried cutting out gluten.
I cut out dairy.
Then caffeine.
Then sugar.
Then life.
I meditated.
I tracked my triggers.
I took probiotics.
I cried in the bathroom.
I canceled plans.
I did everything “right” — and I still had IBS.
And one day, I stopped trying to fight it.
That moment didn’t come out of defeat — it came out of compassion.

Why “Doing More” Isn’t Always the Answer
Many people — including doctors — think IBS is about control. Control your stress. Control your food. Control your mind.
But IBS isn’t a condition that always behaves predictably. Even with the best strategies, symptoms may flare for reasons you can’t explain.
You start to feel like your body is failing. Or worse — that you are.
But it’s not your fault.
You didn’t fail.
You’re not weak.
You’re human.
And sometimes, what the body needs most isn’t another restrictive protocol — it’s permission to rest.
The Science Behind Acceptance
Research in psychosomatic medicine shows that chronic illness acceptance is associated with:
- Lower perceived symptom severity
- Improved quality of life
- Reduced anxiety and depression
- Increased treatment adherence
Acceptance doesn’t mean “giving up.”
It means no longer living in resistance.
In fact, studies on Acceptance and Commitment Therapy (ACT) show it can significantly improve outcomes in IBS by helping patients reduce symptom-related anxiety and avoidance behaviors.
What Changed When I Stopped Fighting
When I stopped obsessing over controlling IBS, here’s what I noticed:
- I stopped fearing every meal
- I could enjoy moments without guilt
- My nervous system felt calmer
- My gut flared less, not more
And ironically, my digestive health improved — not because I added a new treatment, but because I softened my inner world.
What Helped Me Get There
- Journaling without judgment — not food tracking, just feeling tracking
- Eating gently, not perfectly
- Choosing rest over restriction
- Trying probiotics again — this time with curiosity, not desperation
- Working with a specialist who validated my experience, not just my symptoms
One that finally introduced me to spore-based probiotics, which supported my gut in a way nothing else had.
If You’re Tired, You’re Not Alone
If you’re exhausted from the endless IBS cycle, I see you.
And I want to remind you:
You don’t have to “win” against IBS to live well.
You don’t have to be symptom-free to feel peaceful inside your body.
You’re not broken. You’re adapting.
And sometimes, letting go is what allows the healing to begin.

If you’re ready to support your gut gently, and you’re open to a new kind of microbiome support, explore the benefits of Liquid Spore Probiotic from GutShields — designed for sensitive systems like yours.
-
 Health8 năm ago
Health8 năm agoAll About Microscopic Colitis: Causes, Diagnosis, and Treatment
-

 Entertainment8 năm ago
Entertainment8 năm agoI Tried Medication, Diets, and Meditation — And Finally Found Peace in Acceptance
-

 Health8 năm ago
Health8 năm agoWhat Is a Gastroenterologist? When to See One, and the Problems They Can’t Help With
-

 Health8 năm ago
Health8 năm agoTop 7 Questions to Ask Your Gastroenterologist!
-

 Health8 năm ago
Health8 năm agoWhat Causes Mucus in Your Stool—and Why You Shouldn’t Ignore It
-

 Health8 năm ago
Health8 năm agoA New Cause and Treatment for Lymphedema
-
 Health8 năm ago
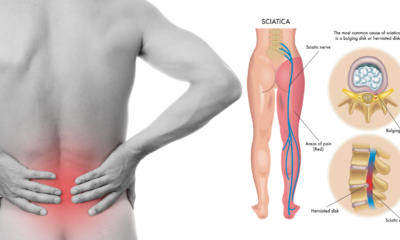
Health8 năm agoIBS and Sciatica Pain – Is There a Connection?
-

 Tech8 năm ago
Tech8 năm agoHealing IBS Isn’t About Forcing Your Gut—It’s About Resetting Its Natural Rhythm
















